This manual provides a comprehensive guide to perioperative management in cardiac surgery‚ encompassing preoperative assessment‚ intraoperative techniques‚ postoperative monitoring‚ and long-term rehabilitation. It integrates current guidelines and evidence-based best practices for optimal patient outcomes and efficient resource utilization. The aim is to standardize care and improve patient recovery.

Preoperative Assessment and Risk Stratification
Thorough preoperative assessment is crucial for optimizing outcomes in cardiac surgery. This involves a detailed medical history‚ including prior cardiac events‚ medications‚ and comorbidities. A comprehensive physical examination should assess cardiovascular function‚ respiratory status‚ and overall health. Essential investigations include electrocardiography (ECG)‚ chest X-ray‚ and blood tests to evaluate renal and hepatic function‚ coagulation parameters‚ and complete blood count. Cardiac imaging‚ such as echocardiography or cardiac computed tomography angiography (CTA)‚ may be necessary to assess cardiac structure and function‚ depending on the individual patient’s clinical presentation and planned surgical procedure. Risk stratification involves identifying patients at high risk for perioperative complications‚ such as myocardial infarction‚ stroke‚ or renal failure. This is accomplished using validated risk scores‚ such as the Revised Cardiac Risk Index (RCRI)‚ incorporating patient-specific characteristics and clinical data to estimate the likelihood of adverse events. Preoperative optimization of medical conditions‚ such as hypertension‚ diabetes‚ and chronic obstructive pulmonary disease (COPD)‚ is essential to minimize perioperative risks and improve outcomes. This may involve medication adjustments‚ lifestyle modifications‚ and specialist consultations to ensure patients are in optimal condition for surgery.
Perioperative Cardiovascular Management
Perioperative cardiovascular management focuses on maintaining hemodynamic stability and minimizing cardiac complications throughout the surgical journey. This begins with careful fluid management to optimize preload and avoid fluid overload or dehydration. Intraoperative monitoring includes continuous ECG‚ arterial blood pressure monitoring‚ and pulse oximetry to detect any hemodynamic instability. Invasive hemodynamic monitoring‚ such as pulmonary artery catheterization‚ may be used in high-risk patients. Blood pressure and heart rate should be closely controlled‚ and any arrhythmias or ischemic changes should be addressed promptly. Pharmacological interventions‚ such as inotropes‚ vasopressors‚ and antiarrhythmics‚ may be necessary to maintain hemodynamic stability. Careful attention to temperature regulation is crucial to prevent hypothermia‚ which can increase the risk of complications. Postoperative cardiovascular management involves close monitoring of hemodynamic parameters‚ ECG‚ and cardiac biomarkers. Early mobilization and respiratory physiotherapy are important to prevent pulmonary complications. Pain management should be tailored to the individual patient to promote comfort and minimize stress on the cardiovascular system; Continued assessment and prompt management of any cardiovascular complications are essential for a successful recovery.
Enhanced Recovery After Cardiac Surgery (ERAS) Protocols
Enhanced Recovery After Cardiac Surgery (ERAS) protocols aim to optimize the patient’s perioperative experience‚ minimizing stress and promoting faster recovery. Key components include preoperative patient education and optimization of nutritional status‚ often involving nutritional counseling and supplementation. Intraoperatively‚ techniques such as minimally invasive approaches and precise fluid management are employed. Postoperative care emphasizes early mobilization‚ reduced opioid use with multimodal analgesia‚ and early enteral feeding to minimize gut dysfunction. A standardized care pathway ensures consistency and efficiency. The ERAS pathway reduces length of hospital stay‚ enhances patient satisfaction‚ improves functional recovery‚ and decreases the incidence of postoperative complications. Regular assessment and adaptation of the protocol based on patient-specific needs are essential for effective implementation. Multidisciplinary team collaboration is crucial for success‚ involving surgeons‚ anesthesiologists‚ nurses‚ and physiotherapists. The goal is to expedite recovery‚ improve quality of life‚ and reduce healthcare costs.
Intraoperative Management Techniques
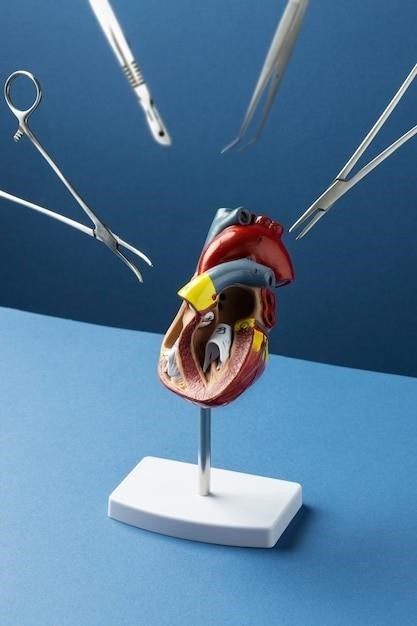
Intraoperative management in cardiac surgery requires meticulous attention to detail and a multidisciplinary approach. Precise surgical technique‚ minimizing trauma and bleeding‚ is paramount. Careful monitoring of hemodynamics‚ including blood pressure‚ heart rate‚ and cardiac output‚ is crucial throughout the procedure. Sophisticated technologies‚ such as transesophageal echocardiography (TEE) and intraoperative neuromonitoring‚ provide real-time assessment of cardiac function and neurological integrity. Maintaining normothermia and appropriate fluid balance helps prevent complications. Blood conservation strategies‚ including cell salvage and meticulous hemostasis‚ are employed to reduce the need for allogeneic blood transfusions. The use of cardiopulmonary bypass (CPB) requires careful management of oxygenation‚ ventilation‚ and temperature control. Post-CPB management focuses on weaning from the bypass circuit and optimizing hemodynamic stability. The choice of surgical approach (e.g.‚ minimally invasive vs. sternotomy) is tailored to the individual patient and the specific cardiac condition. Throughout the operation‚ a vigilant and coordinated team effort ensures patient safety and optimal surgical outcomes.
Postoperative Monitoring and Management
Postoperative care following cardiac surgery is critical for patient recovery and minimizing complications. Continuous monitoring of vital signs‚ including heart rate‚ blood pressure‚ oxygen saturation‚ and urine output‚ is essential in the immediate postoperative period. Pain management is crucial‚ utilizing a multimodal approach to minimize discomfort and promote early mobilization. Careful fluid and electrolyte balance is maintained‚ addressing potential imbalances resulting from surgery and blood loss. Respiratory support may be necessary‚ including mechanical ventilation and close monitoring for respiratory complications such as atelectasis or pneumonia. Cardiac monitoring focuses on rhythm disturbances‚ detecting and treating arrhythmias promptly. Hemodynamic stability is closely watched‚ managing potential hypotension or hypertension. Early mobilization and physiotherapy play a vital role in preventing complications such as deep vein thrombosis (DVT) and pulmonary embolism (PE). Regular assessment of wound healing and potential infections is paramount. Nutritional support is tailored to individual patient needs‚ and dietary adjustments are made to aid recovery and prevent malnutrition. Close monitoring and proactive management of potential postoperative complications are crucial for optimal patient outcomes. Regular assessment and prompt intervention are key to a successful recovery.
Pharmacological Management
Pharmacological management in cardiac surgery encompasses a multifaceted approach aimed at optimizing patient outcomes. Analgesia is crucial‚ often employing a multimodal strategy combining opioids‚ non-steroidal anti-inflammatory drugs (NSAIDs)‚ and regional anesthesia techniques to minimize pain and enhance comfort. Anticoagulation plays a vital role in preventing thromboembolic events‚ with careful selection of agents based on individual patient risk profiles and potential bleeding complications. Inotropic and vasopressor support may be necessary to maintain hemodynamic stability‚ particularly in the immediate postoperative period. Antiarrhythmic medications are used to manage and prevent cardiac rhythm disturbances. Antibiotics are administered prophylactically to reduce the risk of surgical site infections. The management of hypertension and other comorbidities requires careful consideration‚ adjusting medication regimens as needed to optimize cardiovascular function. Beta-blockers may be used to reduce myocardial oxygen demand and improve cardiac stability. Diuretics can help manage fluid overload. Close monitoring of medication effects and potential interactions is critical to ensure patient safety and efficacy. Individualized pharmacological regimens are tailored to specific patient needs and risk profiles‚ balancing the benefits of treatment with potential side effects.
Nutritional Support and Metabolic Optimization
Perioperative nutritional support is critical for optimizing patient outcomes in cardiac surgery. Preoperative nutritional assessment identifies patients at risk of malnutrition‚ enabling timely intervention. Strategies may include nutritional counseling and supplementation to address deficiencies. During the perioperative period‚ maintaining adequate energy and protein intake is paramount to support tissue repair and immune function. Early initiation of enteral nutrition‚ often within 24 hours of surgery‚ is preferred whenever feasible. Parenteral nutrition may be necessary in cases of prolonged inability to tolerate oral or enteral intake. Metabolic optimization focuses on maintaining glucose homeostasis‚ preventing hyperglycemia‚ and minimizing catabolism. Close monitoring of blood glucose levels is essential‚ adjusting insulin therapy as needed. Strategies to reduce inflammation and oxidative stress are employed‚ potentially involving antioxidant supplementation. The timing and type of nutritional support are individualized based on patient factors‚ surgical procedure‚ and recovery progress. A multidisciplinary approach involving surgeons‚ dieticians‚ and nurses is essential for effective nutritional management. Regular monitoring and adjustments ensure that patients receive adequate nutrition to support optimal healing and recovery.
Complications and their Management
Cardiac surgery‚ while life-saving‚ carries inherent risks of complications. Postoperative bleeding‚ requiring potential reoperation or blood transfusions‚ is a major concern. Meticulous surgical technique and vigilant monitoring are crucial for early detection and management. Infection‚ including mediastinitis‚ is another significant risk‚ demanding prompt antibiotic therapy and potentially surgical debridement. Arrhythmias‚ ranging from atrial fibrillation to heart block‚ are common and managed with medication or‚ if necessary‚ pacing. Acute kidney injury can occur due to reduced renal perfusion or nephrotoxic medications; close monitoring of renal function and appropriate fluid management are essential. Respiratory complications‚ such as pneumonia or acute respiratory distress syndrome (ARDS)‚ necessitate respiratory support and meticulous pulmonary hygiene. Neurological complications‚ including stroke or cognitive dysfunction‚ are serious concerns; preventative measures and prompt treatment are crucial. The management of these complications often requires a multidisciplinary approach‚ involving cardiologists‚ intensivists‚ infectious disease specialists‚ and nephrologists. Early detection and prompt intervention are key to improving patient outcomes and reducing mortality.
Long-Term Follow-up and Rehabilitation
Post-discharge care is paramount for optimal recovery and long-term well-being after cardiac surgery. Regular follow-up appointments with the cardiothoracic surgeon and other specialists are vital for monitoring healing‚ addressing any lingering complications‚ and managing medication regimens. Cardiac rehabilitation programs play a crucial role in restoring physical function‚ improving cardiovascular fitness‚ and enhancing quality of life. These programs typically involve supervised exercise‚ education on lifestyle modifications‚ and psychological support. Patients are educated on recognizing and managing symptoms‚ adhering to prescribed medications‚ and adopting a heart-healthy lifestyle‚ including dietary changes and regular physical activity. Psychological support is crucial to address anxiety‚ depression‚ or other emotional challenges that may arise following surgery. Regular monitoring of cardiac function‚ including echocardiograms and electrocardiograms‚ is essential to detect any potential issues early. Long-term follow-up may also include monitoring for recurrence of the underlying cardiac condition or development of new complications. The goal of long-term follow-up and rehabilitation is to help patients regain their independence‚ improve their overall health‚ and maximize their quality of life after cardiac surgery.
Current Guidelines and Recommendations
Staying abreast of the latest guidelines and recommendations is crucial for optimal perioperative cardiac surgical care. The American Heart Association (AHA)‚ American College of Cardiology (ACC)‚ and other multi-society guidelines provide comprehensive recommendations for perioperative cardiovascular management‚ encompassing risk stratification‚ assessment‚ and treatment strategies. These guidelines are regularly updated to reflect the latest scientific evidence and clinical practice. Key areas covered include preoperative optimization of cardiac function‚ intraoperative monitoring and management‚ and postoperative care protocols. Furthermore‚ the European Society of Cardiology (ESC) and other international organizations contribute significantly to establishing global standards of care. Adherence to these guidelines‚ along with integration of evidence-based best practices‚ ensures the delivery of high-quality‚ patient-centered care. Clinicians should regularly review and implement updated guidelines to maintain the highest standards of cardiac surgical care and improve patient outcomes. Continuous professional development and participation in relevant conferences and workshops are vital for staying informed about evolving best practices.